THE 4 STEPS OF THE SCARRING PROCESS*
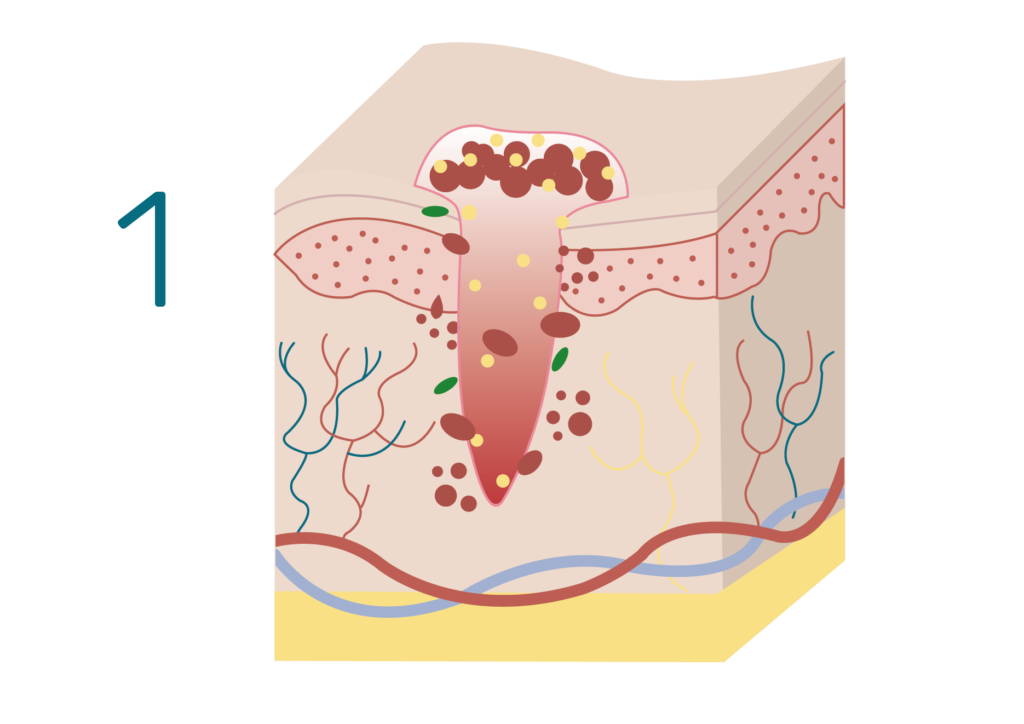
HEMOSTASIS
HEMOSTASIS
During hemostasis, blood vessels contract and platelets form a plug to stop bleeding. Inflammatory molecules and growth factors (proteins that stimulate the growth of specific tissues) are then produced to orchestrate the healing and repair process of the skin.
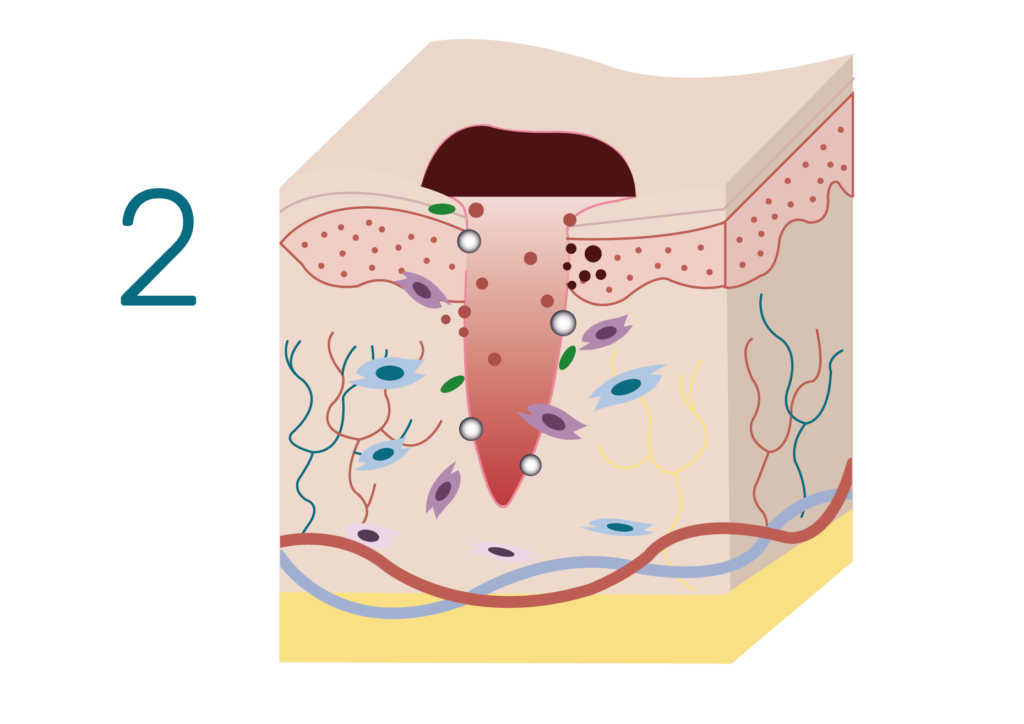
INFLAMMATION
Inflammation
During inflammation, cytokines, molecules and growth factors orchestrate the molecular activities that lay the foundation for scar formation. This process activates the production of collagen and elastin, two vital components for damaged tissues’s reconstruction. While collagen acts as a structure and ensures the good resistance of the tissue, elastin is essential to ensure elasticity of the scar, and helps prevent an overly rigid scar.
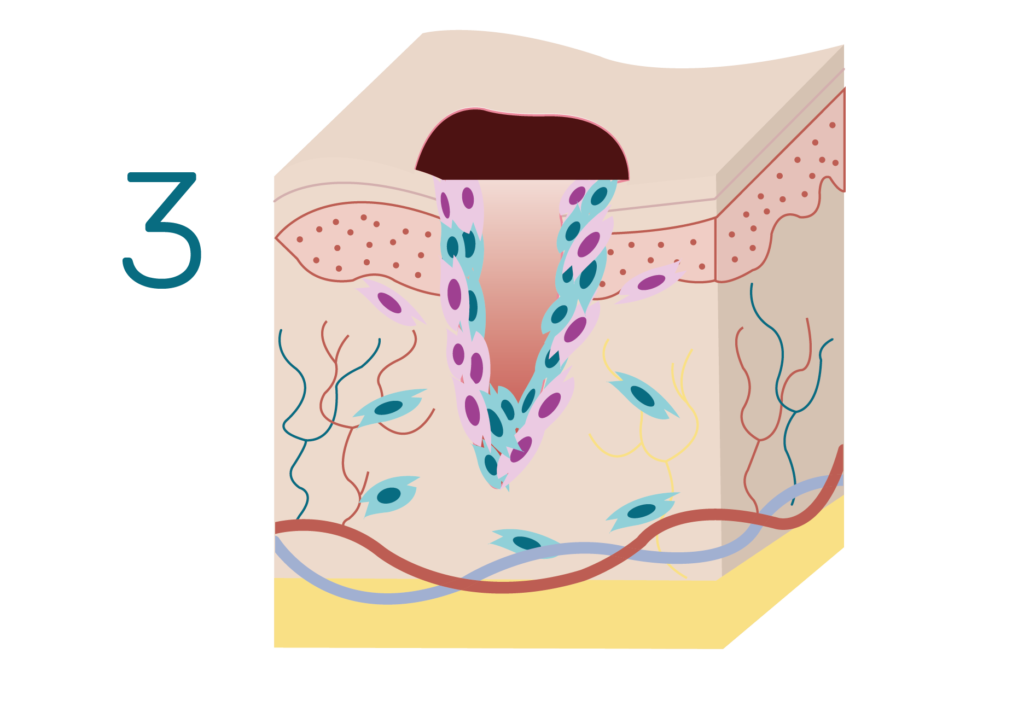
PROLIFERATION
Proliferation
The reconstruction of the tissue then further accelerates as cells further multiply themselves.
In order to obtain an aesthetic and sufficiently elastic scar, the concentration of the molecular healing actors must be appropriately regulated. Indeed, growth factors are key to ensure a good balance between the synthesis of ::
– Collagen Type I, which is thicker and more rigid, and thus essential to restore the extra-cellular matrix
– Collagen Type III, which also contributes to restoring the extra-cellular matrix, but is a lot thinner and flexible than Collagene Type I, and hence essential to make the scar aesthetic and elastic.
– Elastin, which, as Collagen Type III, also participates to ensure the elasticity of the scar.
An imbalanced production between Collagen Type I and III, (overproduction of type I collagen), does not allow the scar process to take place in optimal conditions. In this case, there is a significant risk of getting an unsightly scar such as: a hypertrophic scar, a keloid scar, or other problematic scar symptoms.
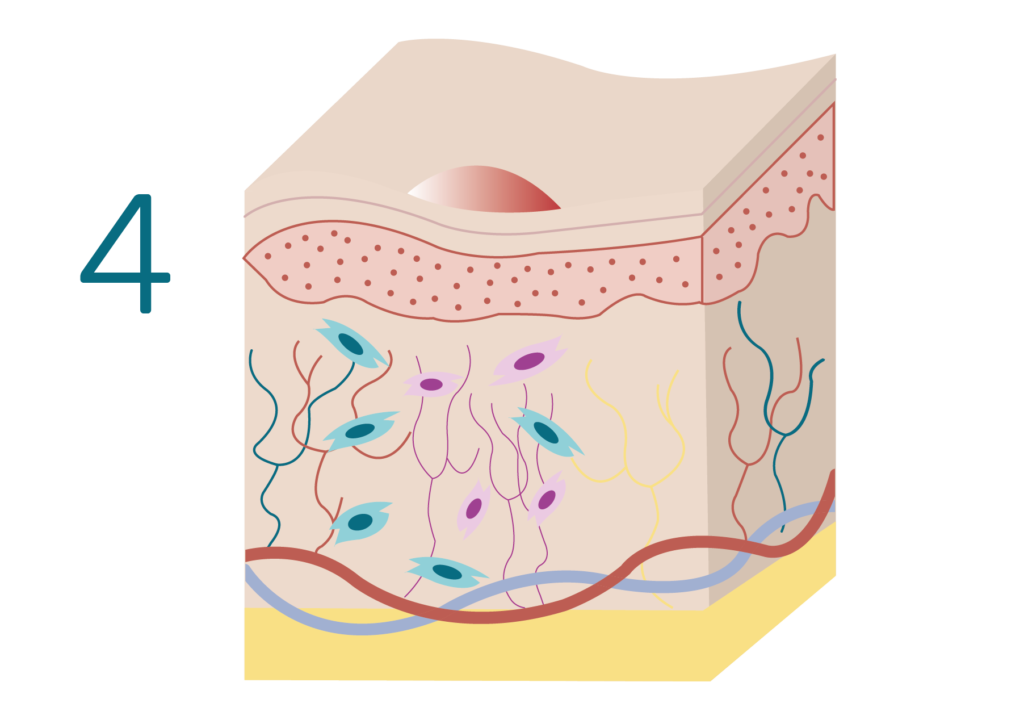
MATURATION
Maturation
During maturation, scar tissue formed during the proliferation phase undergoes structural and organizational changes to strengthen and improve its functionality. Collagen fibers in the scar tissue continue to reorganize and strengthen, while vascularisation gradually decreases. The scar usually becomes flatter, softer and paler over time. This process can take several months to several years depending on the characteristics of the original wound and on the individuals.
Potential scarring difficulties

Hypertrophic SCAR
Symptoms:
- elevated
- red
- thick
Hypertrophic scars*
How are they caused?
The healing process is disrupted which induces an imbalanced production of Collagene Type I and Collagene Type III. Indeed, instead of producing a flat, smooth scar, the body produces an excessive amount of collagen type I, resulting in a raised, lumpy, reddish scar. On contrary to keloid scars, they stay within the boundaries of the original wound and do not extend beyond it.
Factors such as genetics, type and location of the injury, and an overactive healing response contribute to their development. The risk of developping a hypertrophic scar therefore varies accross individuals, as well as for a given individual depending on its surrounding environment.
What do they look like?
Hypertrophic scars are visibly elevated above the surrounding skin, creating a raised or thickened texture.
These scars often appear red or pink, making them more noticeable than the surrounding skin.
Are there any associated symptoms?
Hypertrophic scars may be accompanied by persistent itching, which can be bothersome and contribute to discomfort. Some individuals may experience tenderness or pain at the site of the hypertrophic scar, especially during the early stages of its formation.
It’s important to note that while these symptoms are characteristic of hypertrophic scars, individual experiences may vary. Seeking medical advice is recommended for proper diagnosis and appropriate management of hypertrophic scars.
*Wang ZC, et al. The Roles of Inflammation in Keloid and Hypertrophic Scars. Front Immunol. 2020 Dec 4

Keloid SCAR
Symptoms:
- elevated & overflowing original wound
- shiny & smooth
- itching, tenderness, or pain
Keloid Scars*
How are they caused?
The formation of keloids involves an abnormal response to the healing process, where there is an overproduction of collagen which can grow outside the boundaries of the original wound.
Factors like genetics and skin tension play a role in their development. The risk of developping a keloid scar therefore varies accross individuals, as well as for a given individual depending on its surronding environment.
How they look like?
Keloid scars have a raised and overgrown appearance, and unlike hypertrophic scars, extend beyond the original wound. These scars often have a shiny and smooth surface, differentiating them from the surrounding skin, and can vary in color from pink to dark brown.
Are there any associated symptoms?
Keloid scars may cause persistent itching, leading to discomfort and some may experience tenderness or pain at the site of the scar.
It’s important to note that while these symptoms are common, individual experiences may vary. Seeking medical advice is recommended for a proper diagnosis and appropriate management of keloid scars.
*Wang ZC, et al. The Roles of Inflammation in Keloid and Hypertrophic Scars. Front Immunol. 2020 Dec 4

Atrophic scar
Symptoms:
- sunken or depressed
- loss of tissue volume
- lighter than surrounding skin
Atrophic scars**
How are they caused?
Atrophic scars occur when there is insufficient collagen (both Type I and Type III) production during the wound healing process. This scars can be caused by conditions such as acne, surgical incisions, or injuries, and they may be more common in individuals with a genetic predisposition to problematic scars. The risk of developping a atrophic scar therefore varies accross individuals, as well as for a given individual depending on its surronding environment.
How they look like?
Atrophic surgical scars appear sunken or depressed compared to the surrounding skin. They are characterized by a loss of tissue volume in the scar area.
Are there any associated symptoms?
Atrophic surgical scars themselves typically do not cause symptoms such as pain or itching.
It’s important to note that while these symptoms are common, individual experiences may vary. Seeking medical advice is recommended for proper diagnosis and appropriate management of hypertrophic scars.
**Connolly D, Vu HL, Mariwalla K, Saedi N. Acne scarring‐pathogenesis, evaluation, and treatment options. J Clin Aesthet Dermatol. 2017

Scarring symptoms
Diverse array of symptoms:
- Pain
- pruritus (itching)
- Loss of sensation in the scar area
Scarring symptoms***
Pain and pruritus (itching) are common symptoms experienced during the scarring process:
– Pain can result from nerve damage during injury or surgery, inflammation, or tension on the skin.
– Pruritus, or itching, can occur as a result of the healing process and the formation of new tissue.
– La perte de sensations
Both pain and itching can be exacerbated by factors such as dryness, tight clothing, and environmental irritants. While these symptoms often diminish over time as the scar matures, they can persist for months or even years in some cases. Various treatment options, including topical creams, silicone gel sheets, massage therapy, and laser therapy, can help alleviate pain and itching associated with scars.
Besides that, loss of sensation in the area of the scar can occur due to damage to nerve endings during the initial injury, surgical procedure, or inflammation. The extent of sensory loss can vary depending on the severity of the wound and the individual’s healing process. In some cases, sensation may return gradually as the nerves regenerate and the scar matures. However, in other instances, particularly with deeper wounds or surgical procedures, permanent loss of sensation may occur.
It’s important to note that while these symptoms are common, individual experiences may vary.It is recommended to consult a doctor for a solid diagnosis and proper management of the symptoms associated with healing.
***Farrukh O, Goutos I. Scar Symptoms: Pruritus and Pain. 2020 Dec 8. In: Téot L, Mustoe TA, Middelkoop E, et al., editors. Textbook on Scar Management: State of the Art Management and Emerging Technologies [Internet]. Cham (CH): Springer; 2020. Chapter 10.
*Velnar T, Bailey T, Smrkolj V. The wound healing process: an overview of the cellular and molecular mechanisms. J Int Med Res. 2009 Sep-Oct
